|
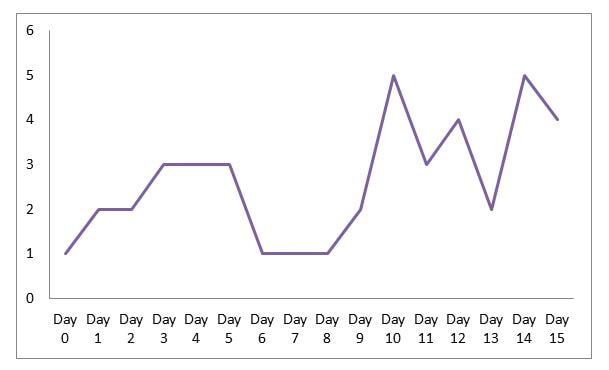
If you are a woman in the United States, you’ve either had a hysterectomy, will have one or know someone who has. I joined thousands of other women on November 26th when I underwent a hysterectomy (uterus/cervix removal) due to suspected adenomyosis and other issues. A salpingectomy (surgical removal of fallopian tubes), single oophorectomy (removal of one ovary) and endometriosis removal was also performed. Hysterectomy is so commonplace in the U.S., and now that it can be performed on an outpatient basis, the seriousness and full recovery time is often downplayed. You will hear about women returning to work 2 weeks after surgery. You will hear stories of little to no pain or complications. It’s truth for those women. You will also hear about women who were couch-bound for weeks, as well as women who had to go back in for revision surgery due to complications. No surgery and no recovery is going to be exactly the same. Even if you have a complication-free surgery and are fit going into it, a smooth recovery is not guaranteed. It doesn’t mean that those who have a bumpy recovery did anything wrong. My surgeon told me that I’d start to feel awesome after just a few days. Well, it’s been just over two weeks and I am only now starting to feel anything resembling “awesome”…and that’s only immediately upon getting up in the morning. As you know, I work with women as a personal trainer/coach. One in three will have a hysterectomy by age 60. For that reason, I’m sharing my experience. When we share our stories, what it does is, it opens up our hearts for other people to share their stories. And it gives us the sense that we are not alone on this journey.” - Janine Shepherd The Day Prior Surgeon’s instructions will determine what actions must be taken the day before surgery. I didn’t have to undergo bowel prep but I did have to limit my intake to clear fluids for the full day. I kept my mind off of this by teaching my last Jazzercise class, washing my sheets, vacuuming, and getting out a few Christmas decorations. I had soup in the crockpot and overnight oats in the fridge. I sustained myself on broth, jello, Gatorade, tea, and water. By the evening, it was clear that my body wasn’t happy with my activity level and lack of food. This resulted in one of the worst headaches of my life. I wanted to go to bed but had to take a shower with the antibacterial soap. I called it a night just before 9 pm. I’ve since decided that I never want to eat jello ever again! Surgery Day I got up before the 4:30 am alarm to take the required morning shower with the same antibacterial soap. My headache subsided sometime during the night. The surgery was scheduled to be outpatient so I pulled on a pair of oversized men’s lounge pants and an Old Navy sweatshirt, knowing I’d need comfortable clothing for the ride home. I had packed a small bag that included paperwork and insurance/id card, water and snacks for my husband, magazine, and phone charger. We arrived at the hospital at just before 5:30 am as instructed. I was my surgeon’s first case of the day: a robotic-assisted laparoscopic hysterectomy. Check-in and Pre-op Pre-op involved last minute tests (last pregnancy test of my life), questions repeated over and over, a few pills, and a few needle sticks. Then it was time to say goodbye to my husband as they rolled me to the pre/post-op holding area. The anesthesiologist, my doctor, and a nurse all visited me in succession after a short wait. Finally, the “2-cocktail” drug compelled me to goofy chatter as I was rolled into the OR. I didn’t have a care in the world. Recovery Room I woke up freezing. My mouth felt like cotton has been stuffed into it. My throat was sore and my voice hoarse. I vaguely remember being wheeled into the private recovery room. It was mid-morning and I expected to be going home by early afternoon. Three criteria had to be met first: pain managed by a pill, no excessive vomiting, and ability to urinate. The crackers I’m asked to eat turned to glue in my mouth. It feels like they turned off my salivary glands during surgery… and I soon discovered that’s not the only part of me that won’t work: the first attempt to urinate = nothing. We repeated the process over and over and each time out of bed was quite the production. Any time I had to move a lot, I was struck by waves of dizziness, nausea, and teeth-chattering shivering. Someone had to help with the IV bag, the vomit cup, and a blanket around my shoulders. I requested some hot tea thinking it’d warm me and help me go. As I shivered like a Chihuahua while sitting on the toilet, my husband kept uttering, “You poor thing.” I promptly vomited tea into the cup. Still no pee. Soon, all that stood between me and going home was the ability to urinate. Every trip to the toilet triggered a wave of shivering and dizziness but no urine. We tried verrrrry slow walks down the hallway, a different bathroom, blowing bubbles in a cup, slow deep breaths (which were quite painful thanks to an air bubble under my rib cage), a warm squeeze bottle, sniffing peppermint, and more. The pressure continued to build but it didn’t matter. At 5 pm, I had no choice. The nurse inserted a catheter as I lay in the hospital bed. I might have let some tears slip. It wasn’t that painful but I felt so vulnerable and disappointed. I’d be staying the night. I soon learned that urinary retention after hysterectomy is one of the most common complications. Overnight Stay My room was in the DCU; it was small but private. The dinner brought to my bedside looked pretty good. I managed to eat the salad, green beans (my favorite) and a little of the chicken and potatoes. My husband left for the night to care for the dogs waiting at home. The first night was the most painful but I was honestly more annoyed by the itchiness from my neck down my torso. Every time I started scratching, I had to take care not to bump the thick square bandage taped to my belly button or the two small incisions near my hip bones. The next morning the catheter was removed, followed by slow walking and unfruitful trips to the bathroom. Four hours was all I got and my bladder just wasn’t ready. Another catheter was inserted but at least this time I was on my way home. Home Sweet Home I had everything I needed within reach, including a lidded cup with a straw that my husband dutifully kept filled with water (a must for pain-free post-surgery hydration). I’m fortunate to have a bed that allows me to recline; normal sleeping positions were not doable at this point. Pain was manageable. I only needed to take my prescription pain meds on Wednesday and Thursday night. Of course, I was not pain-free but the overall pain level wasn't much worse than the pain I'd endured on a regular basis due to the conditions that led me to have surgery. It mostly hurt when I breathed deeply, laughed, or coughed. One silver lining: I didn’t have to get up to go pee. I had been instructed to go to Urgent Care to have the catheter removed on Friday. That afternoon, we took a very uncomfortable ride to the hospital in the pouring rain. I used the online “save my spot” option to limit our time in the waiting room. The catheter was removed and I nervously walked to the bathroom. The tinkle in the toilet was the most wonderful sound! After bladder scans, I was sent home catheter-free. However, now I have to get up to go the bathroom every 30 minutes or so due to awful bladder pressure, which is a common side effect of surgery and having a catheter (or three)...it was uncomfortable but at least it was a small step toward normalcy. Saturday and Sunday were restful other than the trips to the bathroom. Things were looking up! Then on Sunday night at 2 am, I got up to go to the bathroom. Pain seared my right side and I felt dizzy. As I sat on the toilet, I started to hear ringing in my ears, my vision blurred, and a familiar feeling swept over me: I knew I was about to pass out. I made my way down to the cold bathroom tile and pressed my face to it. I called for my husband but he sleeps like the dead. After what felt like an eternity of listening to blood rush in my ears and feeling waves of nausea, I slowly crawled to where he could hear me. I don't think he actually understood what was going on but he helped me back up into bed after making sure I was okay. The next morning, I called the doctor’s office but apparently this is another somewhat common post-op occurrence. I spent most of Monday in bed due to dizziness. Tuesday, December 3rd marked one week since surgery. My husband returned to work so I was on my own but that was okay because I was feeling so much better! Deceived again: as the day wore on, the heaviness and pain in my pelvis and bladder increased. The bathroom trips became more frequent and the discomfort became pain. Uh oh. Urinary tract infections are common after catheter placement and I likely had one. At this point, I was not yet released to drive. Thankfully, my mom had planned to visit me on Wednesday so she took me to the doctor’s office to confirm the infection and get my prescriptions. I started to have pain in my left kidney so I’m grateful to not have waited any longer. Within a few days of being on antibiotics, I started feeling better. I’m now just over two weeks into recovery. I’m feeling better overall but my body regularly reminds me of the fact that I had surgery. A couple of relatable quotes from the HysterSisters Forum: "You feel okay until you don't." "It feels like I was kicked in the crotch by a football player wearing steel-toed boots." My biggest takeaways so far:
0 Comments
Leave a Reply. |
Archives
June 2023
Categories
All
|



 RSS Feed
RSS Feed